A Breakdown of BRCA: The Breast Cancer Gene
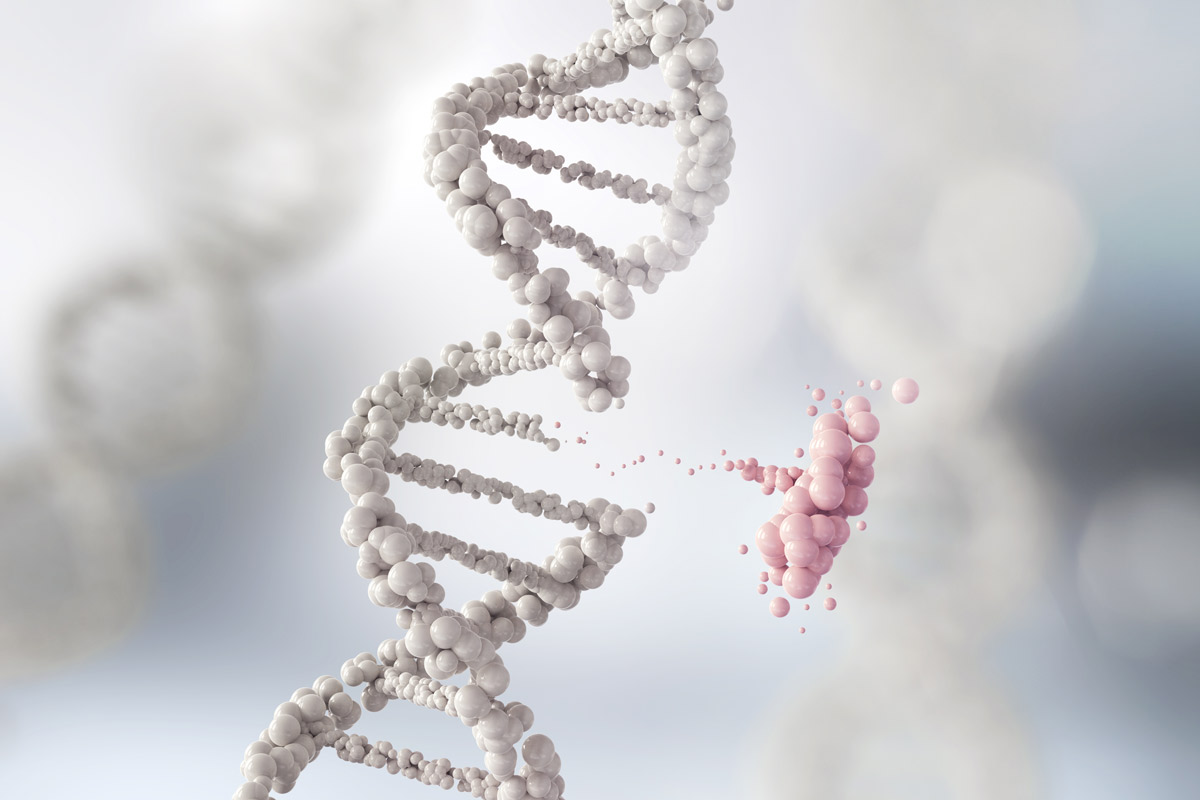
BRCA stands for "breast cancer gene" and refers to two different genes – BRCA1 and BRCA2.
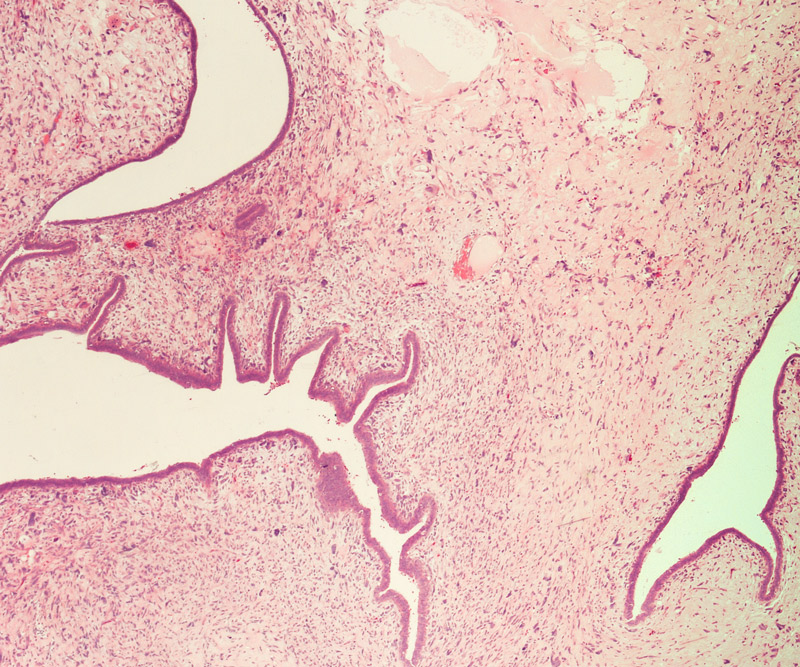
These genes actually are known as "tumor suppressor genes" because of the role they play in helping to repair DNA breaks that can lead to cancer.
The reason why BRCA1 and BRCA2 have gotten a negative rep is because when they are altered or broken – something that occurs in about 0.25% of the population – they are no longer effective at doing their job and have been found to impact a person’s risk for developing breast cancer.

"BRCA1 and BRCA2 are the most common genes mutated in breast cancer," says Dr. Jami Fukui, a breast medical oncologist at Kapiolani Medical Center for Women & Children.
While it is estimated that one in eight women, or 12%, will be diagnosed with breast cancer in her lifetime, that number jumps to 50-85% of women with the BRCA1 mutation who will develop breast cancer before age 70.
That risk is similar in women with the BRCA2 mutation.
"BRCA1 and BRCA2 can lead to hereditary breast and ovarian cancer syndrome, but there are other high-risk genes that are known cancer-susceptibility genes," Fukui says.
"Only 5-10% of breast cancers are linked to a known inherited genetic change. As we learn more, there may be new genes discovered that can put someone at increased risk of developing breast cancer, so it's important that if you have had genetic testing to check in every three to five years to see if there are any updates," she says.
Having the BRCA mutation not only increases a person’s risk for developing breast cancer, it elevates the chance for developing other types of cancers, including ovarian, pancreatic and even prostate cancers.
That's right – men can be impacted by the gene as well.
Though male breast cancer is rare and makes up approximately 1% of breast cancer cases, any man who develops breast cancer should consider genetic testing.
"BRCA1 and BRCA2 are inherited in an autosomal dominant way, meaning the abnormal gene can be passed from one parent and cause disease," Fukui explains. "It is important that men test if they have a breast cancer susceptibility gene, as it may have implications for themselves and their children."
Fukui also recommends both women and men schedule a standing annual wellness exam with their primary care physician to make sure there have not been any changes in their health over the past 12 months.
Women who are at average risk should also have a screening mammogram every year starting at age 40.
However, those who have an increased risk, such as those who test positive for BRCA1 or BRCA2, should begin mammography screening earlier.
"Early detection is so important," Fukui says. "Most breast cancer, when caught early, can be cured."

Studies suggest other factors can reduce a woman's risk for developing breast cancer, including:
- Eating a heart-healthy diet.
- Being physically active for at least 30 minutes daily.
- Not smoking.
- Breastfeeding and having children.
If you do test positive for the BRCA gene, Fukui recommends following up with a support group, which can provide recommendations for various types of screening – not only for breast cancer, but for other cancers as well. They can also discuss medications that can help reduce someone's risk of developing breast cancer, as well as risk-reducing surgery options for prevention.
To learn more about cancer screenings, treatment options and support programs available at the Hawaii Pacific Health Cancer Centers, click here.
Published on: October 11, 2019