What is Non-Alcoholic Fatty Liver Disease?
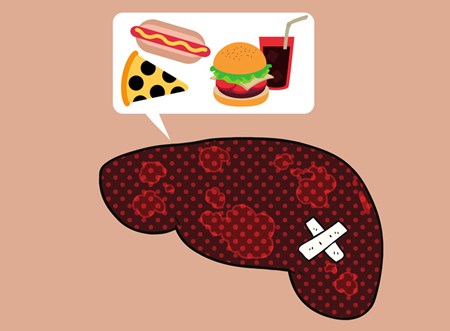
Non-alcoholic fatty liver disease, or NAFLD, refers in general to fat buildup in the liver.
Between 80 million and 100 million Americans are estimated to have NAFLD, making it the most common cause of liver problems in the United States.
As obesity rates climb, so has the rate of NAFLD – in the past 20 years, the number of patients diagnosed with the disease has doubled.
However, it is unclear how many people have NAFLD because most individuals experience no symptoms.
What is NAFLD?
There are two main types of NAFLD:
- Non-alcoholic fatty liver (NAFL) – Fatty deposits are seen in the liver but without any surrounding inflammation. NAFL is generally found accidentally, such as when a person has imaging tests of the abdomen for unrelated reasons. Liver function is normal, and the person has no symptoms.
- Non-alcoholic steatohepatitis (NASH) – Fatty deposits are seen along with liver inflammation, which makes NASH more worrisome than NAFL. Liver function testing may be abnormal, with elevated levels of liver enzymes. There also may be the presence of scar tissue, otherwise known as fibrosis. If untreated, fibrosis from NASH can worsen and even result in liver cirrhosis.
How Do I know if I am At Risk for NASH?
The most common conditions associated with an increased risk of NASH include the following:
- Obesity – More than 70% of individuals with NASH suffer from obesity.
- Type 2 diabetes – Approximately 75% of people with NASH also have Type 2 diabetes.
- Hyperlipidemia, especially high triglycerides.
- Metabolic syndrome – Individuals with metabolic syndrome are at elevated risk for heart disease and diabetes, and tend to gain more weight easily but have difficulty losing. This can include patients who have abnormal levels of blood sugar (not necessarily diabetes), blood pressure and cholesterol, plus a tendency to gain weight around the middle of the body.
- Drugs and poisons – Exposure to certain medications (including amiodarone, tamoxifen and steroids) along with some pesticides has been linked to NASH. However, this is more unusual than the above four conditions.
If you have one or more of these conditions, you may wish to discuss screening with your primary care physician.
Diagnosing NASH
NASH is most often found by accident during routine blood tests.
Tests may show high levels of liver enzymes – particularly alanine aminotransferase (ALT) and aspartate aminotransferase (AST).
If abnormal enzymes are found, doctors sometimes recommend additional testing, such as a liver ultrasound, CT scan or MRI.
A liver biopsy is sometimes also recommended to rule out the presence of a different liver problem.
As a biopsy alternative, a liver fibroscan is sometimes recommended. Fibroscan is a specialized type of ultrasound to look specifically at how much liver scarring is present from NASH, which can help your doctor understand how severe the problem is.

What Can I Do If I Have NASH?
First and most importantly, work on weight loss.
Losing weight quickly reduces liver enzyme levels and allows the liver to start to heal.
It is important to use a well-formulated diet that includes adequate (not high) protein.
The help of a registered dietitian is essential.
In addition, as many people with NASH have metabolic syndrome, weight loss can help improve this condition and reduce your risk of heart disease.
Avoid alcohol, as this can worsen liver disease.
Also, avoid excess amounts of Tylenol, which can aggravate the liver in high doses.
Do not take over-the-counter supplements without discussing with your physician, as many supplements can have unintended side effects on the liver.
Finally, get vaccinated for liver-impacting preventable diseases such as influenza, pneumonia, HPV and hepatitis A, B and C. This simple step can help reduce the risk of additional stress on the liver.
Published on: November 2, 2018