Learn more about our
Info Sessions
toll-free
808 951 LOSS (5677)
Surgical Options
Promotion of Weight Loss with Bariatric Surgery
The surgical techniques that result in weight loss work primarily by limiting how much food the stomach can hold. They are often combined with another type of procedure, a gastric bypass, which limits the calories and nutrients that get absorbed from food.
Gastric banding, gastric bypass and vertical-banded gastroplasty are surgeries that limit the amount of food the stomach can hold by closing off or removing parts of the stomach. These are called “restrictive” procedures. These surgeries also slow down the speed at which the stomach digests food.
Most patients who have restrictive surgeries feel full and satisfied after eating a small amount of food. They also don’t feeling excessively hungry most of the time. After having these surgeries, people can only eat about a quarter-cup of food at a time. Eating more than that is uncomfortable and may result in vomiting.
Gastric bypass is a surgery that creates a direct connection from the stomach to a lower segment of the small intestine, bypassing the first two parts of the small intestine. This procedure causes food to be poorly digested and absorbed, reducing the calories the body absorbs as well as the nutrients. After having this surgery, people must make a lifetime commitment to take vitamin and mineral supplements and eat a high-protein diet to prevent malnutrition.
Although the results of surgical weight loss procedures are predictable and manageable, side effects can persist for some patients.
Restrictive Procedures
These weight loss procedures limit the size of the stomach so that you feel full after eating very small meals, and you eat much less. The weight loss that results from restrictive procedures is not as drastic as the weight loss that results from malabsorptive procedures and gastric bypass; however, they have less risk of malnutrition. Restrictive procedures can be accompanied by a considerable amount of vomiting.
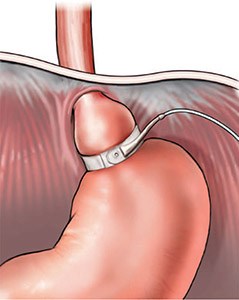
The LAP-BAND® system places an adjustable band at the top of the stomach to create a pouch. The opening from the pouch to the rest of the stomach is adjustable through a small port that rests beneath the skin. The LAP-BAND is a reversible procedure.
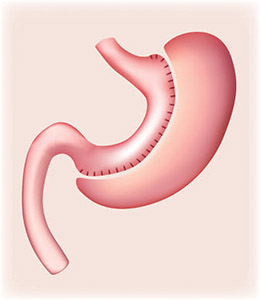
The Vertical Sleeve Gastrectomy is a surgery that removes around 80 percent of the stomach. The new, smaller stomach is the shape of a banana. This procedure does not bypass the intestines, so food is digested and absorbed properly in the intestines. This surgery removes the ghrelin hormone, which significantly reduces the feeling of hunger. This procedure is not recommended for people with GERD, as it may cause pre-existing symptoms to worsen.
Malabsorptive Procedures
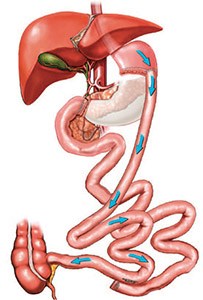
Biliopancreatic diversion and duodenal switch (dS) is more effective in achieving excellent weight loss for people who are extremely obese, but it has a higher rate of malnutrition. Malnutrition is rare for those who undergo gastric bypass. The dS procedure removes about two-thirds of the stomach. It also connects the first part of the small intestine to the third part of the small intestine (skipping the second part of the intestine), so that food moves more quickly through the small intestine. As a result, the body absorbs fewer calories but also fewer nutrients. This procedure has a far lower risk of liver problems, stomach ulcers and dumping syndrome than with other malabsorptive procedures.
Combination Procedures
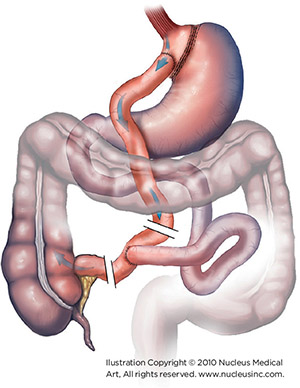
The Roux-en-Y gastric bypass is a restrictive procedure that also results in malabsorption due to bypassing food around the first two sections of the small intestine, the duodenum and the initial part of the jejunum. It carries similar risks as vertical-banded gastroplasty, including pouch stretching, breakdown of the staple lines and leakage of stomach contents into the abdomen. However, because gastric bypass causes food to skip the duodenum, where most iron and calcium are absorbed, risks for nutritional deficiencies are higher. Anemia may result from malabsorption of vitamin B12 and iron in menstruating women, and decreased absorption of calcium may result in osteoporosis and metabolic bone disease. Patients are required to take lifelong nutritional supplements that usually prevent these deficiencies.
The risks of gastric bypass include dumping syndrome, in which the stomach contents move too rapidly through the small intestine, causing nausea, weakness, sweating, faintness and, sometimes, diarrhea after eating. It is also possible that eating sweets will cause weakness, sweating and light-headedness.
Roux-en-Y Gastric Bypass
This procedure can be done with open surgery or by laparoscopy, depending on the individual’s needs. Surgical techniques may vary.
- Exploration of the abdomen – A small incision or a set of laparoscopic openings are made and the surgeon checks to see if there are any anatomical abnormalities. Particular attention is given to the gallbladder, uterus and ovaries. If the gallbladder contains any gallstones, it will be removed later in operation. (When this surgery is done via laparoscopy, an ultrasound is done before surgery to check for gallstones and a separate procedure is scheduled to remove them.)
- Creating the roux limb – The small intestine is separated 15 to 40 centimeters down from the ligament of treitz, which is where the second section of the small intestine (called the jejunum) begins. A length of the jejunum is measured out to create a “roux limb” that will be attached to the stomach. The standard roux limb is about 75 centimeters long. Sometimes a longer roux limb is made for heavier patients.
- Dividing the stomach – The stomach is cut to create a tiny stomach pouch, about 15 to 20 milliliters in size, just below the esophagus. This is done with a tool that divides the tissue and seals the tissue on each side of the cut with staples
- Forming the gastro-jejunal anastomosis – The new stomach pouch is attached to the new roux limb. This step is a key step in the surgery. The “hookup” must have excellent blood supply and must not have any tension remaining on it at the completion of the operation. A stapling device is used to create this connection.
- Final procedures – Depending on a person’s individual needs, the surgeon may also remove the gallbladder (cholecystectomy), tie off the fallopian tubes (tubal ligation), take a liver biopsy, or place a stomach tube (gastrostomy). The surgeon usually places a plastic drainage tube near the site of the “hookup” to watch for leaks in this area and to aid in therapy if a leak occurs.
- Closing up – Whether a larger incision for open gastric bypass or several small incisions for the laparoscopic gastric bypass were made, the muscle is closed with stitches that will be absorbed by the body. The skin is then closed with suture, steri-strips® or staples, depending on the surgeon’s preference.
What to Expect
Surgical Options

— Maria Ver, MD, Bariatric Surgeon, Pali Momi 360° Weight Management Center


